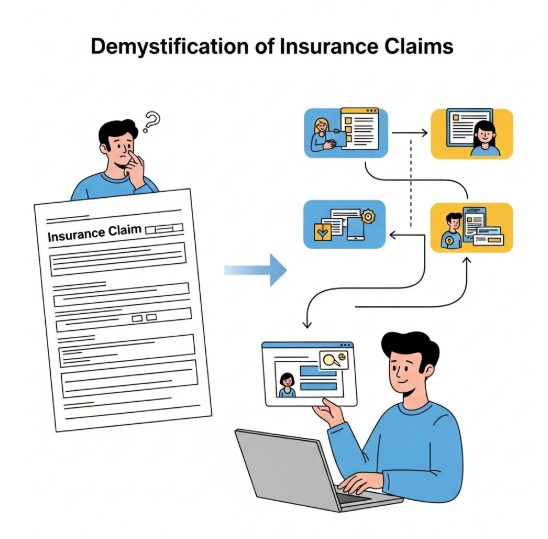
The processes in the claims process are usually the same for both manual and computerized submissions. Payer-specific claims procedures differ, but the overall framework outlined below explains how the system should function.
Submission of a claim: A psychologist can manually or electronically file a claim to a health plan. While paper claims are scanned or inputted into the computer system, electronic claims are translated or transformed into a standard format. When you send a claim to a billing service or clearinghouse, for example, the intermediary usually handles the claim and sends it to the payer.
Claims adjudication: Following its entry into the business’s computer system, the claim data undergoes a procedure known as “claims adjudication.” By comparing the claim to the health plan’s coverage and benefit requirements, the business determines whether the claim is legitimate. All of the information required to initiate payment is verified in the claim.
Adjudication notification: The practice usually receives an explanation, sometimes known as a “remittance advice,” outlining the adjudication process’s conclusion. A “explanation of benefits” detailing the services rendered and the manner in which the funds have been received is also usually issued to the covered customer and the practice.
When a claim receives approval, the company processes payment to the practice. Should the practice engage a third party like a billing service, the health plan might direct payment to that service, which will then transfer the funds to the practice. There may be instances where a claim is approved but only partially compensated; in such cases, the payer is obligated to provide an explanation.
If the claim is suspended, the practice may be requested to refile the claim with further details.
In the event that the claim is rejected, the practice or the intermediary can initiate an appeal.
Payment and tracking: There may be a range in the amount of time that passes between filing a claim and getting paid. In general, processing electronic claims is far faster than processing paper claims. Using a billing service or clearinghouse has several advantages, including the ability for these middlemen to monitor claims until they are paid, which aids in the prompt identification and resolution of issues. Practices without a middleman can call or visit the company’s website to find out the status of claims.